Recognizing LEMS
The early recognition of LEMS is crucial for improving clinical outcomes but remains a major challenge.
—Merino-Ramírez et al, 20161
The early recognition of LEMS is crucial for improving clinical outcomes but remains a major challenge.
—Merino-Ramírez et al, 20161
Lambert-Eaton myasthenic syndrome (LEMS) is an autoimmune disorder of the neuromuscular junction.6 It causes debilitating and progressive muscle weakness and fatigue, the effects of which leave patients with diminished physical functioning and a poorer quality of life.1,3,6,7 And, while it is considered a rare disease—at least 3,600 individuals in the US are affected—it is estimated that about half of these individuals are still undiagnosed.4,7 They suffer despite the fact there are simple tests available to clinicians that can accurately diagnose the disorder and effective medicines that can mitigate its devastating effects.4
By becoming more “LEMS aware,” you may be better equipped to recognize the disorder and expedite the treatment journey for patients.
About LEMS
Pathophysiology of LEMS
Patients with LEMS experience severe muscle weakness due to reduced acetylcholine (ACh) release from presynaptic motor nerve terminals.8
- Approximately 50%-60% of LEMS cases are associated with cancer4
- LEMS symptoms can appear ≥5 years before, after, or at the time of cancer diagnosis9
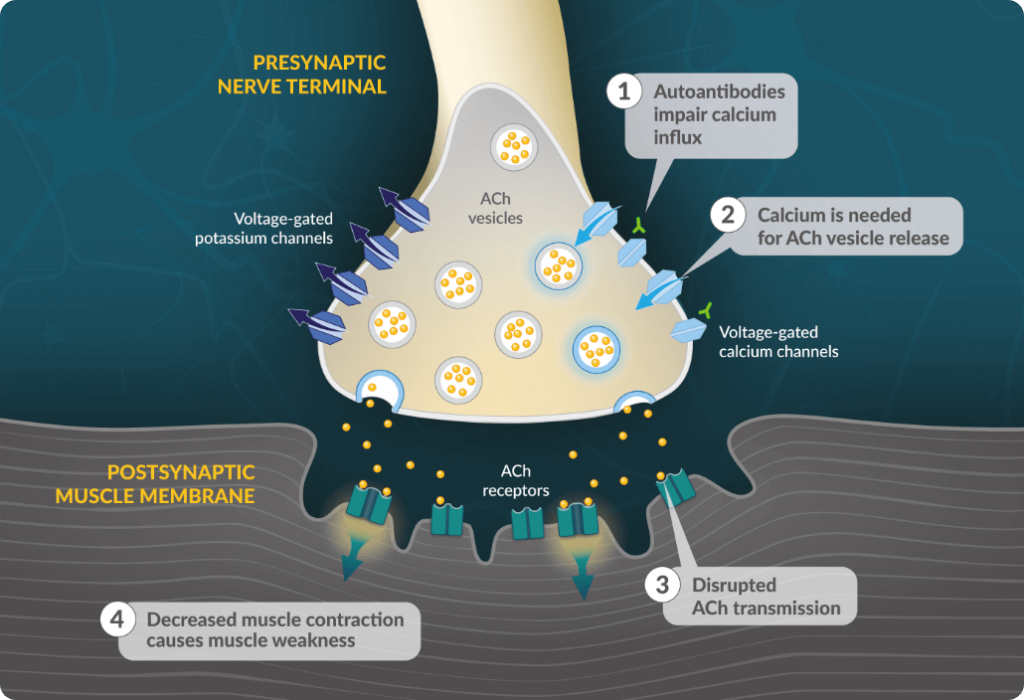
- In patients with LEMS, autoantibodies target voltage-gated calcium channels on the presynaptic motor neuron, reducing calcium influx during an action potential8
- Reduced intracellular calcium limits presynaptic vesicle fusion and release of ACh8
- Disrupted ACh transmission lessens activation of ACh receptors on the muscle fiber potential8
- Reduced ACh signaling results in diminished muscle fiber contraction and muscle weakness8
Progression of LEMS
LEMS is progressive and debilitating and may contribute to a high level of disease burden, which can worsen over time3,4
In a 2012 study of patients living with LEMS3:
75% reported partial or total restriction in activities of daily living3, such as rising from a chair or climbing stairs10
50% reported severe leg weakness; other frequently reported symptoms included dry mouth and visual difficulties3
Based on EQ-5D scores*, the
health-related quality of life for
LEMS patients is comparable
to multiple sclerosis3
*A measure that generates a single index value for health status with considerable potential for use in healthcare evaluation.
In a 2001 study, ~25% of LEMS patients required a wheelchair all of the time or for mobilization outside of the home.11
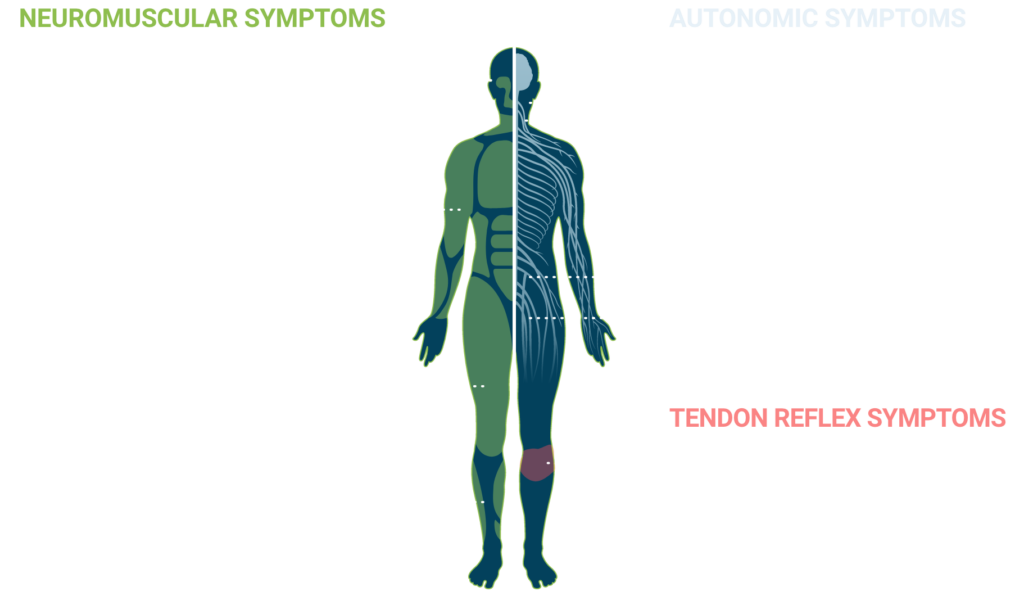
Symptoms of LEMS
The progressive nature of LEMS and the diagnostic challenges that it presents make early symptom recognition critical for optimal patient care.
Presentation of LEMS
LEMS is often suspected based on a clinical triad of signs and symptoms4:
Proximal muscle weakness
Autonomic symptoms (eg, dry mouth, impotence)
Hyporeflexia or areflexia
The LEMS Gait
LEMS gait
“Waddling” is a classic symptom seen in many patients with LEMS prior to treatment. In this video, you will see an example of a patient’s use of extending their arms outside of a normal range, leaning side to side while tilting their pelvis, and swinging a leg to compensate for a compromised balance while walking.
LEMS Pop Quiz
In addition to proximal muscle weakness, what other LEMS signs or symptoms would you need to see before ordering a diagnostic antibody test for your patient?
(Select all that apply)Because many patients with LEMS spend an average of 4.4 years searching for a correct diagnosis3, proximal muscle weakness is reason enough to order a LEMS antibody test for your patients.
The presentation of areflexia/hyporeflexia—and autonomic symptoms such as dry mouth, dry eyes, constipation, and impotence—only adds to the urgency to test for LEMS. And with the availability of a free anti-VGCC antibody test from Catalyst, there’s no reason to delay testing that can help identify patients struggling with symptoms of LEMS.
Insights from a LEMS expert
Mazen M. Dimachkie, MD, FAAN, FANA, a Professor
of Neurology at The University of Kansas Medical
Center, discusses one often-misdiagnosed cause of
weakness and fatigue: LEMS.
Within this video presentation, Dr. Dimachkie walks
through determining the cause of a patient’s muscle
weakness, common clinical symptoms, and
diagnostic testing in order to help clinicians
diagnose LEMS. Excerpts from this presentation
appear throughout this website, and you can watch
the full webinar here.
3 QUESTIONS TO ASK YOUR PATIENTS
If you suspect a patient may have LEMS, here are 3 questions to ask that can help advance the conversation.
Do you or does anyone in your family have a history of autoimmune disorders?
In LEMS not associated with cancer, pre-existing autoimmune conditions are frequently observed4. Examples include hypo- and hyperthyroidism, celiac disease, type 1 diabetes, ulcerative colitis, Addison’s disease, and rheumatoid arthritis. Like many other autoimmune disorders, a genetic susceptibility may be present in LEMS not associated with cancer.9,12
Do you have a history of smoking and/or unexplained weight loss?
In addition to advanced age, a history of smoking and unexplained weight loss are independent predictors of paraneoplastic LEMS.12
Where did your muscle weakness begin, and how did it spread?
Another differentiating feature of LEMS may be the direction of symptom spread. In LEMS, symptoms typically start in the lower body and spread upward, while symptoms of myasthenia gravis—a more common neuromuscular junction disorder—typically start in the face/neck and spread downward.1
Take the lead on LEMS
Use this simple wordplay to help remember the clinical triad of signs and symptoms that should point to a suspicion of LEMS.