The Link Between LEMS and Cancer
Overall, the median time between onset of LEMS and cancer diagnosis was 6 months and ranged between 6 years before and 5 years after cancer diagnosis.
—Wirtz et al, 20029
Overall, the median time between onset of LEMS and cancer diagnosis was 6 months and ranged between 6 years before and 5 years after cancer diagnosis.
—Wirtz et al, 20029
The benefits of earlier diagnosis of Lambert-Eaton myasthenic syndrome (LEMS) include limiting disability along with loss of muscle function, mobility, and quality of life for patients. But for more than half of patients afflicted with LEMS, the benefits of diagnosis are often even more significant.3,4
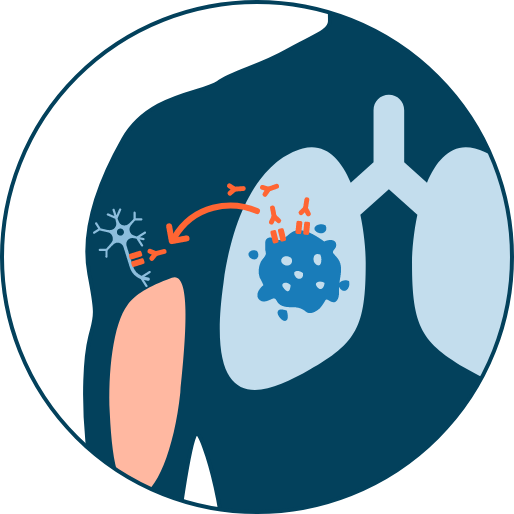
Approximately 60% of LEMS cases are caused by an underlying tumor, typically small cell lung cancer (SCLC).39 The reported median time between onset of LEMS and a subsequent cancer diagnosis is 6 months.9 Patients with LEMS associated with SCLC are more frequently found while still having limited disease.40 With regular screening, most SCLCs can be discovered within 1 year of a LEMS diagnosis.9,41
In this section, we’ll present clinical and practical information that will help you better understand the relationship between these two diseases and how you can use these insights to improve clinical outcomes for your patients.
Insights from a LEMS expert
Mazen Dimachkie, MD, FAAN, FANA, a Professor of
Neurology at The University of Kansas Medical
Center, discusses one often-misdiagnosed cause of
weakness and fatigue: LEMS.
Within this video presentation, Dr. Dimachkie walks
through determining the cause of a patient’s muscle
weakness, common clinical symptoms, and
diagnostic testing in order to help clinicians
diagnose LEMS. Excerpts from this presentation
appear throughout this website, and you can watch the full webinar here.*
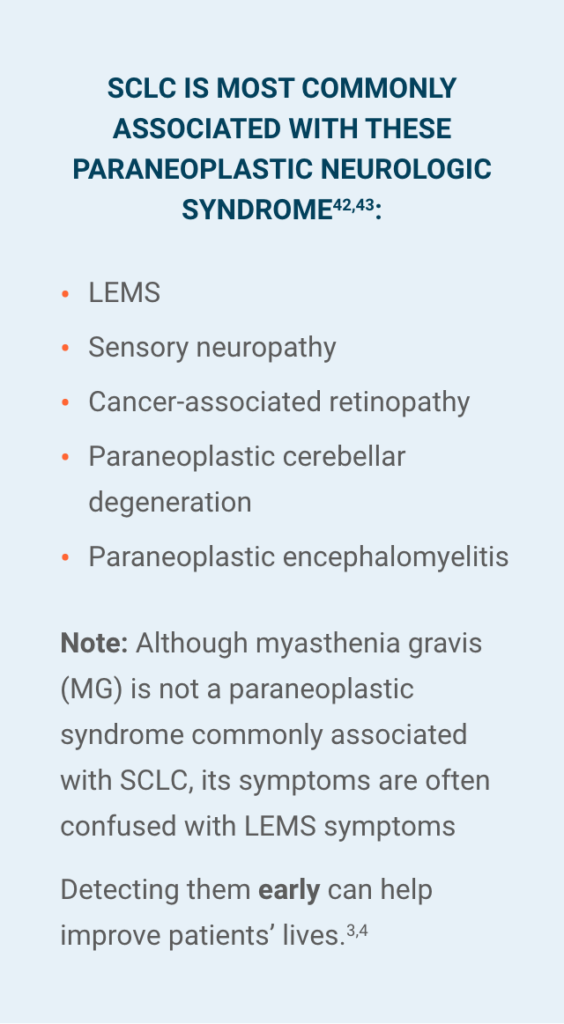
PARANEOPLASTIC SYNDROMES OF THE
NERVOUS SYSTEM
Paraneoplastic syndromes of the nervous system are a heterogeneous group of neurological disorders caused by the immune response to an underlying tumor—specifically, against the onconeural antigen expressed by both the tumor and the nervous system. These syndromes are not caused by cancer metastasis. LEMS is considered a classic example of this syndrome.42
1 in 10 patients with lung cancer develops a paraneoplastic syndrome. 42-44
Suspect your patient may have a paraneoplastic syndrome?
DOWNLOAD THE ONCOLOGY DIAGNOSTIC CHECKLIST.
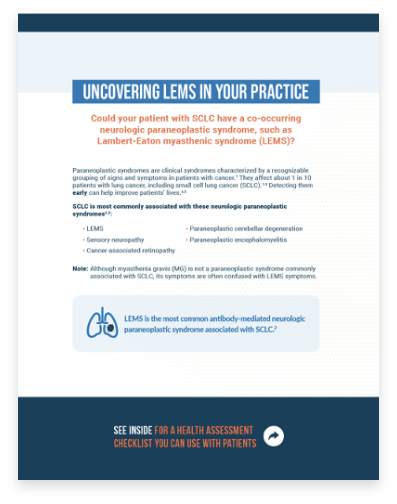
Review the flashcard
Uncovering LEMS In Your Practice.
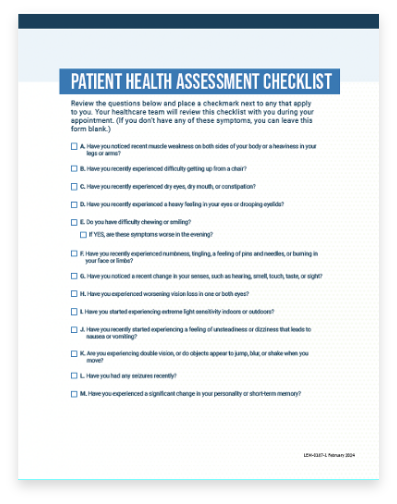
Have your patient
complete the Patient
Health Assessment
Checklist.
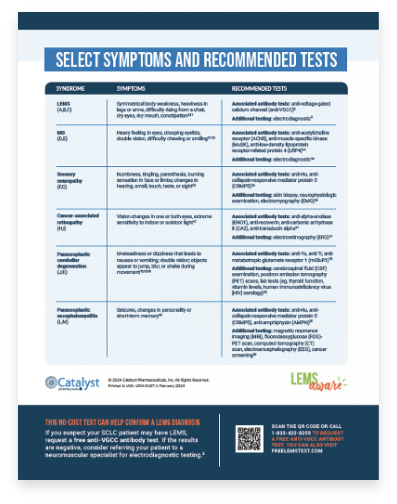
Review results with
your patient and refer to
the Select Symptoms
and Recommended
Tests chart to
determine next steps.
3 categories of paraneoplastic syndromes of the nervous system
Central nervous system44
Examples include encephalomyelitis and limbic encephalitis
Peripheral nervous system44
Examples include subacute sensory neuronopathy and
certain neuropathies
Neuromuscular junction and muscle44
One example of this syndrome is LEMS
THE CANCERS OF LEMS
According to one publication, the cancers most commonly
associated with LEMS9

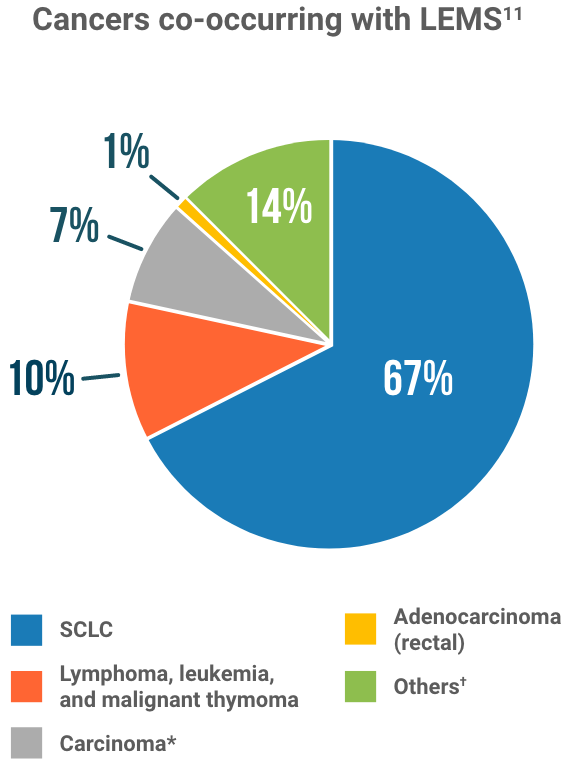
*Carcinoma=prostate, laryngeal, breast, gallbladder, and maxillary glandule.
†Including ameloblastoma or lymph metastasis, with unknown primary. Percentages are approximations.
An evaluation of oncology healthcare claims data between 2017 and 2022 shows that >90% of LEMS cases in SCLC patients may still be undiagnosed46
Review this poster presentation for yourself.
Are LEMS Symptoms Being Masked In Your
Patients With SCLC?
Are LEMS Symptoms Being
Masked in Your Patients
With SCLC?
Are muscle weakness and fatigue in SCLC patients
always a symptom of the malignancy, or could they
be signs of a paraneoplastic syndrome? This video
illustrates how the adverse effects of cancer and
anticancer therapy can mask the symptoms of LEMS.
INSIGHTS FROM A STUDY OF LEMS ASSOCIATED WITH SCLC
In a Neurology 2020 observational study, “Long-term follow-up, qualify of life, and survival of patients with Lambert-Eaton myasthenic syndrome,” Lipka et al detail the findings of 150 patients with LEMS—54% related to small cell lung cancer (SCLC).40
Key insights from this study include40:
- Rates of cancer survival
- Progression of LEMS symptoms
- Impact of LEMS on quality of life
- Results of treatment of LEMS symptoms using immunosuppressive and neuromuscular junction-modulating therapies
Study design40
- Observational study using data collected between July 1998 and October 2015
- 150 patients diagnosed with LEMS, based on characteristic clinical features and confirmed by either the presence of antibodies to voltage-gated calcium channels, or specific patterns on low frequency repetitive nerve stimulation and on high frequency repetitive nerve stimulation
- 59% of patients (n=85) had an associated lung cancer
Progression of LEMS
- 73% of LEMS patients used a mobility-assistance device at some point during the course of disease (median follow-up time: 12-130 months)40
- 52% used a wheelchair, and 6% were fully wheelchair-dependent at any point during their disease course42
- Patients with LEMS associated with SCLC reported more functional impairment course vs patients with LEMS without SCLC40
- Median time from onset of LEMS symptoms to diagnosis was 18 months in patients without SCLC vs 4 months in patients with SCLC40
- Median time from onset of LEMS symptoms to maximum disease severity was 12 months for LEMS not associated with SCLC vs 4 months in patients with SCLC40

Quality of life
- Surviving subjects participated in a 36-question survey to determine their Health-Related Quality of Life (HRQoL) with SCLC40
- 8 domains of HRQoL were examined, including physical functions; physical role limitations due to physical problems; bodily pain; general health evaluation; vitality; social functioning; emotional role limitations due to emotional problems; and mental health
- Responses were compiled to produce a physical composite score (PCS) and mental composite score (MCS)
- LEMS patients with and without an SCLC diagnosis reported lower HRQol scores vs the general population, reflected in lower scores in 3 of 4 related PCS domains40
Treatment
- Among patients who received symptomatic treatment with 3,4-DAP or pyridostigmine, 88% reported improvement in symptoms due to 3,4-DAP vs only 67% who reported improvement due to pyridostigmine (N=150)42
- Effects of pyridostigmine may be short-lived
- Patients treated with symptomatic therapy appeared to improve sooner after diagnosis vs those treated with immunosuppressive drugs40

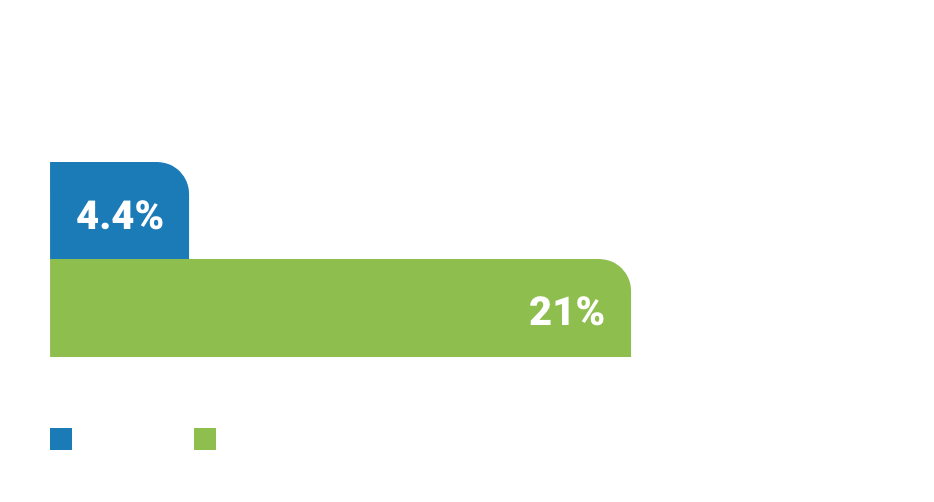
Median survival is doubled in patients with SCLC-LEMS with extensive disease compared to patients with SCLC without LEMS, and overall 5-year survival is increased from 4.4% to 21%.41
—Lipka et al, 2020
LEMS POP QUIZ
Which of the following therapies is recommended for the symptomatic treatment of LEMS whether associated with cancer or not?
(Select all that apply)Amifampridine. Symptomatic treatment of LEMS is recommended in addition to anticancer therapy for patients with cancer-associated LEMS.29 While steroids, IVIG, and pyridostigmine have all been used in limited capacity for the treatment of LEMS, only amifampridine is approved and recommended for LEMS.47,48
Learn more about the use of amifampridine in patients with cancer-associated LEMS.